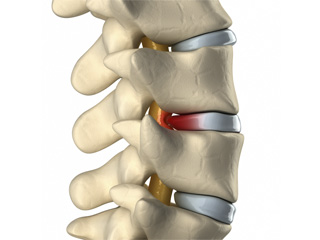
A spinal disc herniation or protrusion affects the invertebral disc structure arising from a degenerative process.
The invertebral disc is made up of two main parts:
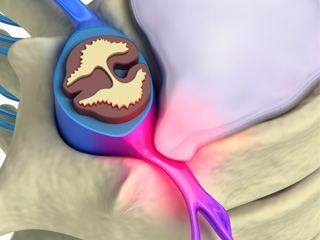
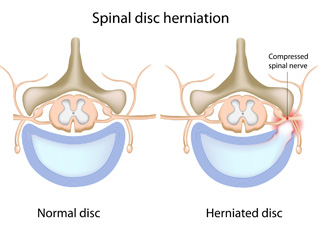
- the inner portion of the disc called nucleus pulposus; it is a soft and jelly-like material composed primarily of water responsible for the cushioning and support of the vertebras.
- the outer part of the disc is a stronger and more fibrous material called the annulus fibrosus that surrounds and contains the nucleus.
A herniated disc occurs when the nucleus pulposus is forced through a weakened part of the disc and bulges out beyond the outer layers. It is due to age related deterioration of the annulus fibrosus, repeated overloads, etc. This fragment compresses the spinal cord and/or nerve roots.
The classic symptom is Sciatica. This pain is due to impingement of one of the nerve roots and it radiates into the parts affected by the irritation. Typically, symptoms are experienced only on one leg, but if the prolapse is quite large and set in a central position, both legs may be affected.
The compression of a nerve root also includes sensory changes. The patient may suffer from numbness, muscle cramps, burning feeling or cold and others. In severe cases, the nerve root is so damaged that causes loss of muscle strength.
There is a disorder particularly serious known as Cauda Equina Syndrome, originated from a large prolapse in a central position. Roots or conus medullaris damage can result in pain, reduced strength in legs, loss of bowel and bladder control and sensitivity loss of the perineum (genital and anal regions).
The most apropriate test to diagnose a disc herniation is the Magnetic Nuclear Resonance (RNM). Although traditional plain X-rays are limited in their ability to image soft tissues, they help to indentify other associated pathologies (scoliosis, spondylolisthesis) that may influence the prognosis and treatment.
Electromyogram/ electroneurogram (EMG/ENG) sindicates whether there is nerve damage and level of harm on roots. It also allows us to make the difference between acute and chronic injuries.
Initial treatment is conservative and it does not require surgery. It usually consists of analgesics, antiinflammatories, muscle relaxants and neuroleptic medication.
Hereafter physical activity should be restricted, absolut rest is not essential, though. When acute phase finishes, physical therapy should be started.In severe cases patients can use an orthosis temporarily (lumbosacral back support).
After 4-6 months of evolution, 90% of spinal disc herniations treated in a conservative way show reasonable to major improvement without surgery. Thus surgery indications are limited and can be summed up in:
- Failure or lack of the conservative treatment efficiency.
- Presence of neurlogical deficit, entendido como loss of muscle strength or abolition of reflexes.
- Presence of Cauda Equina Syndrome is considered a medical emergency requiring immediate attention and surgical procedure.
Surgery
The procedure consists of removing the herniated disc fragment, known as DISCECTOMY. The intervention can be carried out by differents ways depending on the patient's features, prolapse degree, associated vertebral alterations.
For those who just need an isolated discectomy, it can be undertaken by a minimally invasive technique with a small incision.
There are other situations in which “vertebral instability” (caused by arthrosis on a herniated disc, vertebral misalignment) requires a discectomy involving spinal fixation with screws (called SPINAL FUSION). Besides the screws, the spinal fusion can be reinforced with cages filled with bone grafting at the level of the removed disc. These interbody cages have reduced complications stemming from spinal instrumentation.